The field of regenerative medicine has taken a monumental leap forward with the advent of 3D bioprinting technology, particularly in the realm of stem cell applications. Scientists are now harnessing the power of stem cells to construct artificial organs, a breakthrough that could revolutionize organ transplantation and tissue engineering. This cutting-edge approach combines the precision of 3D printing with the regenerative potential of stem cells, offering hope to millions of patients awaiting life-saving transplants.
The Science Behind 3D Bioprinting with Stem Cells
At its core, 3D bioprinting operates on principles similar to conventional 3D printing but with a biological twist. Instead of plastics or metals, bioprinters use bioinks—specially formulated materials containing living cells, growth factors, and biomaterials. Stem cells, with their unique ability to differentiate into various cell types, serve as the building blocks for these bioinks. Researchers can direct stem cells to become specific tissues, such as heart muscle, liver cells, or even neurons, before layering them into complex three-dimensional structures.
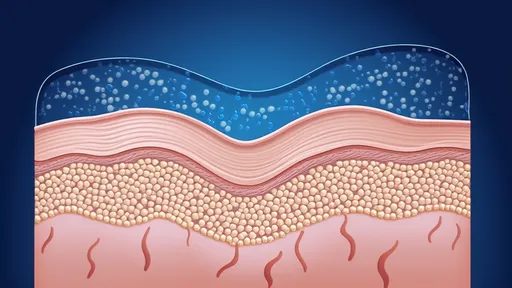
The process begins with detailed imaging of the target organ, often using CT or MRI scans. This digital blueprint guides the bioprinter as it deposits layer upon layer of cell-laden bioink. Advanced bioprinters can create intricate vascular networks within these structures, addressing one of the major challenges in tissue engineering: ensuring adequate blood supply to keep the artificial organ alive.
Recent Breakthroughs in Organ Fabrication
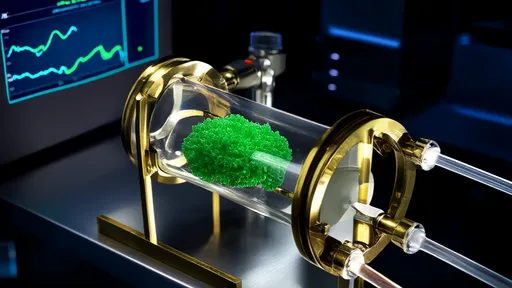
Several research teams worldwide have reported significant progress in creating functional organ constructs. At Wake Forest Institute for Regenerative Medicine, scientists have successfully bioprinted miniature human livers capable of producing albumin and other liver-specific proteins. Meanwhile, a team at Tel Aviv University created the first 3D-printed heart using a patient's own cells, complete with blood vessels, ventricles, and chambers.
Perhaps most remarkably, researchers at Harvard's Wyss Institute have developed a technique called SWIFT (Sacrificial Writing Into Functional Tissue) that allows for the creation of organ-specific tissues with high cell density. Their method involves printing vascular channels into living matrices composed of stem cell-derived organ building blocks, resulting in tissues that more closely mimic native organ function.
Overcoming Technical Challenges
The road to viable 3D-printed organs hasn't been without obstacles. One persistent challenge has been achieving the necessary cell density for functional tissues. Early bioprinted structures often lacked the cellular packing found in natural organs, leading to weak mechanical properties and limited functionality. Newer approaches, such as the use of stem cell spheroids rather than single-cell suspensions, have helped overcome this limitation.
Another hurdle involves maintaining cell viability throughout the printing process. The mechanical stress of extrusion-based printing can damage delicate cells. Researchers have responded by developing gentler printing methods, including laser-assisted and acoustic bioprinting, which can handle sensitive stem cells with greater care.
The immune response presents yet another challenge. Even when using a patient's own stem cells, the artificial organ must integrate with the host's body without triggering rejection. Scientists are exploring various biomaterial coatings and immune-modulating factors to ensure compatibility.
Clinical Applications on the Horizon
While fully functional 3D-printed organs for transplantation remain several years away, the technology is already finding clinical applications. Pharmaceutical companies are using bioprinted human tissues for drug testing, providing more accurate models than animal testing. Burn victims are benefiting from bioprinted skin grafts, and dentists are experimenting with 3D-printed dental tissues.
Perhaps the most immediate impact will be seen in partial organ repairs. Rather than replacing entire organs, clinicians may soon be able to bioprint patches for damaged hearts or segments of diseased livers. This approach could significantly reduce transplant waiting lists by keeping patients healthier longer while they await full organ replacements.
Ethical Considerations and Future Directions
As with any groundbreaking medical technology, 3D bioprinting raises important ethical questions. The use of embryonic stem cells remains controversial in some circles, though the field has largely shifted toward induced pluripotent stem cells (iPSCs), which can be derived from adult tissues. There are also concerns about equitable access to what will likely be an expensive treatment initially.
Looking ahead, researchers aim to scale up the technology to create full-size human organs and improve their longevity and functionality. Some envision bioprinting centers where patients' stem cells are banked and organs are printed on demand. Others speculate about the possibility of enhancing organs beyond natural human capacity, raising philosophical questions about human augmentation.
The convergence of stem cell biology and 3D printing represents one of the most exciting frontiers in medicine today. As the technology matures, it promises to transform our approach to organ failure and tissue damage, potentially saving countless lives and improving quality of life for millions more. While challenges remain, the pace of progress suggests that the era of 3D-printed organs may arrive sooner than we think.

By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025
By /Aug 7, 2025
By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025
By /Aug 7, 2025
By /Aug 7, 2025

By /Aug 7, 2025
By /Aug 7, 2025
By /Aug 7, 2025

By /Aug 7, 2025
By /Aug 7, 2025

By /Aug 7, 2025

By /Aug 7, 2025